It's no surprise that adverts for antacid tablets come into full swing at the same time as the Christmas festivities. For some people, heartburn is an unwelcome, but regular, visitor during the season of good will. Dr Mark Austin, consultant gastroenterologist at The Montefiore Hospital in Hove, explains how to reduce the symptoms and when to seek help.
Read More
Here comes winter and almost everyone seems to have a cough! But if your cough lasts for three weeks or more it could be something more serious than a 'bit of a cold'.
Read More
A diabetes specialist is offering patients advice and the most up-to-date treatment at a private hospital in Hove. Sunil Zachariah 43, has joined the Montefiore Hospital, in Hove, as obesity and, with it, the prevalence of type 2 diabetes increases in the Brighton and Hove area.
Read More
Mike O’Connell is a consultant Ear, Nose & Throat Surgeon who specialises in nasal conditions, sinusitis, cosmetic nose and ear surgery but also many general conditions.
Read More
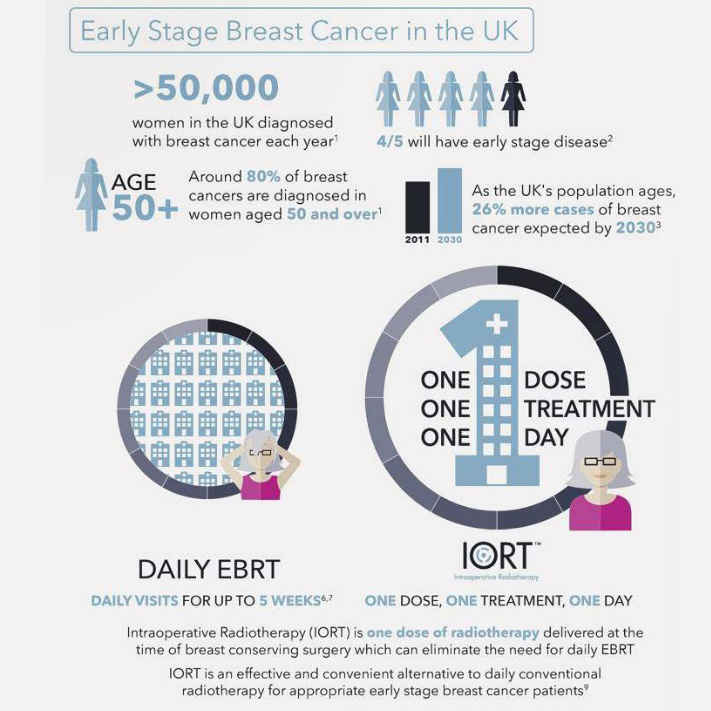
In the South East of England, a patient experience study of 18 early stage cancer patients who opted for single dose intraoperative radiotherapy (IORT), found positive patient reported outcomes for this alternative to standard daily external beam radiotherapy (EBRT).
Read More
Tony Miles, a Consultant General Surgeon who specializes in colorectal surgery, talks about a problem many people find difficult to discuss.
Read More
Mr Goldie Khera, a Consultant General Surgeon who specialises in laparoscopic (key-hole) upper GI surgery, talks about hernias - a common problem which can affect us at any age.
Read More